68.表阿霉素
出处:按学科分类—医药、卫生 军事医学科学出版社《临床常用进口药物手册》第390页(14435字)
【中文释文】:
(表柔比星)
〔说明〕
表阿霉素(表柔比星)是一种新的蒽环类抗生素,具抗肿瘤活性,由Farmitalia Carlo Erba研究室合成。
〔生物活性〕
表阿霉素的作用机制与该药可与DNA结合有关。细胞培养研究表明该药可迅速透入细胞进入细胞核,抑制核酸的合成和有丝分裂。已证实表阿霉素有广谱的抗实验性肿瘤作用,包括L1210和P388白血病,肉瘤SA180(团块型,腹水型),黑色素瘤B16,乳腺癌,路易斯肺癌以及结肠癌38。对移植到无胸腺小鼠的人体肿瘤细胞也有抑制作用。
动物毒性研究表明表阿霉素治疗指数高于多柔比星(阿霉素),而全身及心脏毒性反应较多柔比星低。
〔临床药理学〕
在肝肾功能正常的病人中,按75~90mg/m2给药,血浆水平是以三指数的形式下降,呈现为快速1期和缓慢终末期,其平均半衰期为40h。
药物的主要代谢成分,即13-OH衍生物,其血浆水平一直较低且与药物原形相平行。表阿霉素主要经肝排出,高血浆清除率值(0.9L/min)表明,此药缓慢排出是由于广泛分布于组织中所致。该药不能通过血脑屏障。
〔适应证〕
表阿霉素单一用药对多种肿瘤有广谱的抑制作用,包括乳癌,恶性淋巴瘤,软组织肉瘤和胃癌。
初步研究表明,该药对恶性黑色素瘤,结肠癌也有抗肿瘤活性。
表阿霉素与其他抗癌药联合使用,可用于治疗肺癌和卵巢癌。
〔禁忌证〕
表阿霉素禁用于既往用过抗肿瘤药物治疗或放疗,而造成显着骨髓抑制的病人及已用过大剂量蒽环类药物(如多柔比星或柔红霉素)治疗的病人。
该药禁用于近期或既往有心脏受损病史的病人。
〔剂量〕
表阿霉素单一使用时其成人剂量为60~90mg/m2,静脉注射3~5min注入体内,根据病人骨髓像的情况,上述剂量可间隔21d后重复使用。
小剂量(60~75mg/m2)可用于那些由于早期化疗、放疗、老年,或骨髓新生物浸润而造成骨髓造血功能不良。每一疗程的总剂量可分为2~3个节段日。当该药与其他抗肿瘤制剂合用时应减量。由于表阿霉素的排泄是经肝胆系统,故肝功能不全者应减量,以避免蓄积中毒。中度肝功受损(胆红素14~30mg,BSP滞留量9%~5%)药量应减少50%,而重度肝脏受损(胆红素>30mg,BSP滞留量>15%)药量需减少75%。
中度肾功能受损无需减少剂量,因为,通过肾排出的表阿霉素的量非常有限。
〔注意事项〕
用表阿霉素的病人第一疗程必须细微经常监测。红细胞、白细胞、血小板应认真检查。白血病病人用正常剂量服药,通常有一过性的血细胞下降,用药的10~14d降到最低,21d可恢复至正常。
如可能在治疗开始及治疗过程中应检查肝功能(SGOT,SGPT,碱性磷酸酶,胆红素,BSP)。
动物实验资料和短期人体实验表明表阿霉素的心脏毒性反应较结构类似的多柔比星为小。然而鉴于目前临床应用知识,该药总蓄积量应限制在550mg/m2体表面积。
若连续治疗超过上述蓄积量,则应考虑防止心力衰竭危险的上升以及其他蒽环类化合物所引起的副作用。据报道,心力衰竭可能发生在终止治疗几周后,且用有关治疗无效。纵膈、心包区的肿瘤目前或既往用过放疗的,最大蓄积量应减至400~450mg/m2。
在确定最大蓄积量时,任何有潜在心脏毒性作用的治疗药物,都应计算在内。
每一周治疗前后应行心电图检查。心电图的变化有T波低平或倒置,ST段压低,心律失常,但这种心律失常通常是一过性的,可逆的,无需中止治疗。蒽环类的多柔比星引起的心脏病是一种特殊类型,表现为QRS低电压,收缩间期延长(PEP/VET),射血分数减低。
对于接受表阿霉素治疗的病人来说,心脏监护是非常重要的,可以通过非介入性检查技术检测心脏功能,如心电图,超声心动图,必要时可用放射性核素造影测定射血分数。
和其他细胞毒制剂一样,表阿霉素可以造成高尿酸血症,这是由于肿瘤细胞迅速分解所致,因此为了控制这种情况的发生,认真检查血尿酸的水平是很有必要的。
就目前资料来说,该药对人体繁殖、畸胎及胚胎是否有影响尚无结论性的定论。动物实验资料表明,表阿霉素对胚胎有害。
与其他大多数抗肿瘤药和免疫抑制剂一样在特殊实验条件下,表阿霉素对实验动物有诱发和致癌作用。在用表阿霉素后1~2d可出现尿液变红。
〔副作用〕
除了骨髓抑制和心脏毒性的副作用外,还有如下几种副作用:
1.脱发。60%~90%的病例可出现这种情况,一般是可逆的,男性有胡须生成受抑。
2.粘膜炎。治疗开始后5-10d可出现粘膜炎,一般表现为胃炎伴糜烂,舌两侧及舌下腺炎。
3.胃肠功能紊乱。如恶心、呕吐、腹泻。
4.高热。
5.曾有报道,偶尔发生发热,寒颤,荨麻疹及过敏反应等。
〔用法〕
表阿霉素应静脉给药,口服、肌肉注射、皮下注射无效。检查针头确实在静脉内之后,经通畅的生理盐水输液管内给药,这一方法可减少药物外溢的危险,并确保给药后静脉用盐水冲洗。
表阿霉素注射时溢出静脉外,会造成组织的严重损伤甚至坏死。注射小静脉或反复用同一血管会造成静脉硬化。表阿霉素不可与肝素混合,二者化学性质不配伍,且在特定比率下可能会发生沉淀。
表阿霉素可与其他抗肿瘤制剂合用但不应在同一注射器中混合。
〔溶液的制备〕
表阿霉素可溶于无菌注射用水,其配制如下:
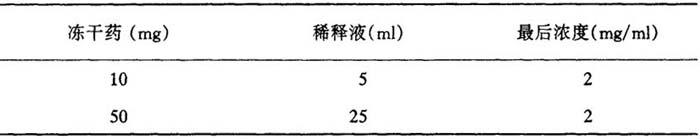
表24 表阿毒素溶液的制备
加入无菌注射用水后,摇动药瓶至药物完全溶解。配制好的溶液在室温下可存放24h,在冰箱内(4~10℃)可存放48h,溶液必须避光。
在接触药品时应戴保护性手套,一旦皮肤或粘膜接触到表阿霉素的粉剂或溶液应用肥皂或清水冲洗,眼结膜应用盐水冲洗。
〔注意〕
表阿霉素应由有抗肿瘤和细胞毒药物治疗经验的医师应用。
最初治疗应有认真的基础监护,包括各种实验室数据和心脏功能。
〔剂型〕
盐酸表阿霉素有两种剂型。
10mg瓶装:内含10mg盐酸表柔比星冻干粉。
50mg瓶装:内含50mg盐酸表柔比星冻干粉。
〔生产厂家〕
意大利爱宝大药厂
(附本品别名:阿表比星,表比星,Farmorubicin,Pidorubicin,IMI28,4-EA,4’-EpiADE,4’-Epi-Doxorubicine)
【外文释文】:
Description
Pharmorubicin(epirubicin hydrochloride)is a new anthracycline antibiotic with antiblastic activity,synthesized in the Farmitalia Carlo Erba Research Laboratories.
Biological activity
The mechanism of action of Pharmorubicin is related to its ability to bind to DNA.Cell culture studies have shown rapid cell penetration,localization in the nucleus and inhibition of nucleic acid synthesis and mitosis.Pharmorubicin has proved to be active on a wide spectrum of experimental tumours including L 1210 and p 388 leukaemias,sarcomas SA 180(solid and ascitic forms),melanoma B 16,mammary carcinoma,Lewis lung carcinoma and colon carcinoma 38.It has also shown activity against human tumours transplanted into athymic nude mice(melanoma,mammary lung,prostatic and ovarian carcinomas).
Toxicity studies in animals have indicated that Pharmorubicin has a better therapeutic index and less systemic and cardiac toxicity than doxorubicin.
Clinical pharmacology
In patients with normal hepatic and renal function plasma levels after iv injection of 75-90mg/m2 of the drug follow a tri-exponential decreasing pattern with a very fast first phase and a slow terminal phase with a mean half-life of about 40 hours.
Plasma levels of the drug’s main metabolite,the 13-OH derivative,are constantly lower and virtually parallel to those of the unchanged drug.Pharmorubicin is eliminated mainly through the liver.High plasma clearance values(0.9 L/min)indicate that this slow elimination is due to extensive tissue distribution.The drug does not cross the blood-brain barrier.
Indications
Pharmorubicin administered as single agent has shown to produce regression in a broad spectrum of tumours including mammary carcinoma,malignant lymphomas,soft tissue sarcomas and gastric cancer.
Preliminary findings indicate that the drug has produced some antitumour activity in malignant melanoma and in advanced colorectal carcinoma.
Given in combination with other antiblastic drugs,Pharmorubicin has induced also a therapeutic response in lung and ovarian cancer.
Contraindications
Phannorubicin is contraindicated in patients with marked myelosuppression induced by previous treatments with other antitumour agents or by radiotherapy,and in patients already treated with maximal cumulative doses of other anthracyclines such as doxorubicin or daunorubicin.
The drug is contraindicated in patients with a current or previous history of cardiac impairment.
Dosage
When Pharmorubicin is used as a single agent,the recommended dosage in adults is 60-90 mg/m2 body area;the drug should be injected iv in 3-5 minutes and,depending on the patient’s haematomedullar status,the dose should be repeated at 21-day intervals.
Lower doses(60-75mg/m2)are recommended for patients whose bone marrow function has already been impaired by earlier chemotherapy or radiotherapy,by age,or by bonemarrow neoplastic infiltrations.
The total dose per cycle may be divided over 2-3 successive days.When the drug is used in association with other antitumour agents,the doses need to be adequately reduced.Since the major route of elimination of Pharmorubicin is the hepatobiliary system,the dosage should be reduced in patients with impaired liver function,in order to avoid an increase in overall toxicity,Moderate liver impairment(bilirubin,1.4-3 mg/100ml,or BSP retention;9-15%)requires a 50%reduction of dose while seveie impairment(bilirubin>3 mg/100 ml or BSP retention>15%)necessitates a dose reduction of 75%.
Moderate renal impairment does not appear to call for dose reduction in view of the limited amount of Pharmorubicin excreted by this route.
Precautions
During the first cycles of treatment with Pharmorubicin patients must be carefully and frequently monitored.
White and red blood cells and platelet counts should be carefully monitored,Leucopenia is usually transient with normal dosage schedules,reaching a nadir between the 10 th and 14th day,but returning to normal values by the 21 st day.
Before starting treatment and if possible during the treatment,liver function should be evaluated(SGOT,SGPT,alkaline phosphatase,bilirubin,BSP).
Experimental animal data and results of short-term trials in man indicate that Pharmorubicin is less cardiotoxic than its structural analogue doxorubicin.
However,in view of the present state of clinical knowledge,it is advisable to limit the total cumulative dose to 550 mg/m2of body area.
The advantages of continuing a treatment exceeding this cumulative dose should be carefully evaluated against the possibility of increasing the risk of heart failure,of the type described for other anthracycline compounds.
This heart failure has been reported as occurring even several weeks after discontinuation of treatment,and may prove unresponsive to specific medical treatment.
In case of concomitant or previous radiation of the mediastinal-pericardial area,the maximal cumulative dose should be lowered to 400-450 mg/m2 body area.
In order to establish the maximal cumulative dose,any concomitant therapy,where potentially cardiotoxic drugs are given,should be taken into account.
It is recommended to carry out an ECG before and after each treatment cycle.Alterations in the ECG tracing,such as flattening of inversion of the T wave,depression of the S-T segment,or the onset of arrhythmias,generally transient and reversible,need not necessarily be taken as indications to discontinue treatment.
Cardiomyopathy induced by anthracyclines,and by doxorubicin in particular,is associated with a persistent reduction of the QRS voltage,prolongation beyond normal limits of the systolic interval(PEP/LVET)and a reduction of the ejection fraction.
Cardiac monitoring of patients receiving Pharmorubicin treatment is highly important,and it is advisable to assess cardiac function by non-invasive techniques such as ECG,echocardiography and,if necessary,measurement of ejection fraction by radionuclide angiography.
Like other cytotoxic agents,Pharmorubicin may induce hyperuricaemia as result of rapid lysis of neoplastic cells.Blood uric acid levels should thus be carefully checked in order to control pharmacologically this phenomenon.
To date there is no conclusive information as to whether this drug may adversely affect human fertility,or cause teratogenic or other harmful effects to the foetus;experimental data, however suggest that Pharmorubicin may harm the foetus.
Its use in pregnancy is therefore not recommended.
Like most other antitumoural and immunosuppressant agents,Pharmorubicin in particular experimental conditions,has mutagenic properties and is carcinogenic in laboratory animals.
Pharmorubicin may impart a red coloration to the urine for l-2 days after administration.
Adverse reactions
Besides myelosuppression and cardiotoxicity(described under Precautions)the following adverse reactions have been described:
·Alopecia,normally reversible,appears in 60-90%of treated cases;it is accompanied by lack of beard growth in males;
·Mucositis may appear 5-10 days after the start of treatment,and usually involves stomatitis with areas of painful erosions,mainly along the sides of the tongue and on the sublingual mucosa.
·Gastro intestinal disturbances,such as nausea,vomiting and diarrhoea.
·Hyperpyrexia.
·Fever,chills and urticaria have been reported occasionally.Anaphylaxis may occur.
Directions for administration
Pharmorubicin should be administered by intravenous injection.
It is not active when given orally and should not be injected intramuscularly or intrathecally.
It is advisable to give the drug via the tubing of a freely-running saline iv infusion after checking that the needle is well placed in the vein.This method minimizes the risk of drug extravasation and makes sure the vein is flushed with saline after the administration of the drug.
Extravasation of Pharmorubicin from the vein during injection may give rise to severe tissue lesions.even necrosis.Venous sclerosis may result from injection into small vessels or repeated injections into the same vein.
Pharmorubicin should not be mixed with heparin as the two substances are chemically incompatible and in certain ratios may precipitate.
Pharmorubicin can be used in association with other antitumour agents,but it is not recommended that it be mixed with these drugs in the same syringe.
Preparation of the solution
Pharmorubicin is dissolved in sterile water for injection as indicated in the table below:
Table 24

After adding the sterile water,shake the vial until the drug has completely dissolved.The reconstituted solution is stable for 24 h at room temperature,and for 48 h in a refrigerator(4-10℃).It should be protected from light.
It is advisable that personnel handling this drug should wear protective gloves.Accidental contact of Pharmorubicin powder or solution with skin or mucosae should be treated immediately by copious lavage with soap and water.The conjunctiva should be washed with saline solution.
Warnings
Pharmorubicin should be administered only under the supervision of qualified physiciansexperienced in antiblastic and cytotoxic therapy.
Initial treatment calls for a careful baseline monitoring of various laboratory parameters and cardiac function.
How supplied
Pharmorubicin hydrochloride is supplied in two sizes:
·10 mg Vial containing 10 mg of epirubicin hydrochloride as a freeze dried powder.
·50 mg Vial containing 50 mg of epirubicin hydrochloride as a freeze dried powder.
Manufacturer
Erba,Ltd.,Italy